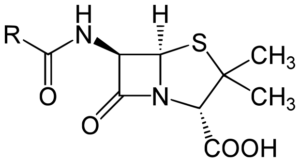
Penicillin, up close and chemical.
When most of us think about bacteria, we think of fairly routine infections that can be cured with a trip to the doctor and a prescription for antibiotics. Unfortunately, this is no longer the case.
Bacterial resistance to antibiotics is quickly rising, and now more than 700,000 people die around the world each year from drug-resistant infections. This past year, a bacterial strain from a Pennsylvania woman was found to carry a gene rendering it resistant to all known antibiotics, including one used only as a last resort in hospitals. There are several reasons for the current drought of viable medications to treat bacterial infections, though none of them are easy fixes. But in a historical turning point mid-September, the United Nations announced that the general assembly has signed a declaration to fight antibiotic resistance and the spread of “superbugs” (bacteria already known to be resistant to current antibiotics).
For scientists who have been worrying about antibiotic resistance for the past 60 years, this comes as a welcome relief to inject more effort and money into a field already under-funded by pharmaceutical companies. But the fight must also reach patients that frequently demand antibiotics and physicians that readily prescribe them for every symptom (i.e., the common cold, which is a viral infection and therefore will not be affected by antibiotics); a JAMA study indicates that approximately 47 million prescriptions for antibiotics are given unnecessarily each year.
The first antibiotic drug, penicillin, was discovered in a happy accident in 1928 when Alexander Fleming found that bacteria would not grow in the presence of a certain type of mold. When formulated into a medication, this molecule became instantly famous as many maladies suddenly became easily treatable. However, it should be noted that even Fleming himself warned of the dangers of drug-resistant bacteria during his 1945 Nobel Prize acceptance speech, but for many years this resistance was not taken too seriously. Though bacteria were beginning to evolve to become resistant to antibiotics, scientists were also moving fast to come up with new antibiotics, and for a period of time in the mid-late 1900s scientists were able to outpace bacteria. But in order to keep up with the costs associated with discovering and producing new drugs, pharmaceutical companies also encouraged doctors to prescribe antibiotics more heavily to drive sales. This increased use of antibiotics therefore increased opportunities for resistance to arise, especially where antibiotics were used incorrectly.
The resistance issue was recognized as far back as the 1960s, though early antibiotic reform proved difficult given the number of parties involved. Pharmaceutical companies discover and produce the drugs but doctors, healthcare administrators, and governments are all responsible for their distribution. Antibiotics are also spread beyond the clinics in the use of livestock, as many farmers have introduced low doses of antibiotics to increase growth in animals.
And yet decreasing the number of antibiotics prescribed and used each day will have little effect on our current “war against superbugs.” In order to battle bacteria head on, we need better antibiotics—drugs that will not only kill bacteria, but make it harder for bacteria to develop resistance. Drug discovery and development is a huge bottleneck in this process, as antibiotics are not especially high-grossing drugs for pharmaceutical companies since they are intended for short term use. This lowers incentives for pharmaceutical companies to spend time and effort developing these drugs when they are unlikely to cover the development costs incurred during the discovery process; research through clinical trials can cost companies over 2.5 billion dollars. But beyond cost, antibiotic development is hard. We have not been able to identify a new class of antibiotics since the 1980s, and not for lack of trying. Thus with the combination of these factors, most major pharmaceutical companies are not currently researching antibiotics. Today less than 40 antibiotics are currently in development, and even fewer will make it through FDA trials.
This lack of effective drugs and resistant bacteria has been widely felt, and not only in the MRSA (methicillin-resistant Staphylococcus aureus) infections that plague hospitals and similar environments. Earlier this year it was reported that syphilis cases have shot up recently around the country. Once thought to be in a category with tuberculosis and polio (diseases rarely seen in the United States), syphilis’ comeback has much to do with modern medicine no longer consistently being an effective treatment. With the current track that we are on, this is undoubtedly not the only disease that will be making a resurgence in the coming years.
And unfortunately, a UN declaration is not going to quickly solve a problem that has been nearly 100 years in the making. But it will force this issue to be part of a political conversation among world leaders, and that is something worthwhile.
