Gut Reactions
February 27, 2025

“Everything is connected,” we often remind one another, nodding wisely—but with no idea of the implications.
Not until the end of the twentieth century did we realize that the immune system’s inflammatory response plays a central role in anxiety, depression, schizophrenia, MS and other auto-immune diseases, Alzheimer’s and other forms of dementia, Parkinson’s, ALS, various forms of autism—the list goes on. Researchers had assumed that the immune system left the brain alone. Instead, it pulls strings.
Now that we realize that much, we can add the next set of connections. Today’s hot research area is the gut microbiome, because it sends the messages that activate (or overactivate) the immune system.
From the gut to the immune system to the brain, a series of reactions unfolds that “may cause, potentiate, initiate or drive” either healing or disease, says Dr. Jonathan Kipnis. “I sound vague,” he adds, “because we don’t yet know enough. If we knew everything, there would be no need for a center!”
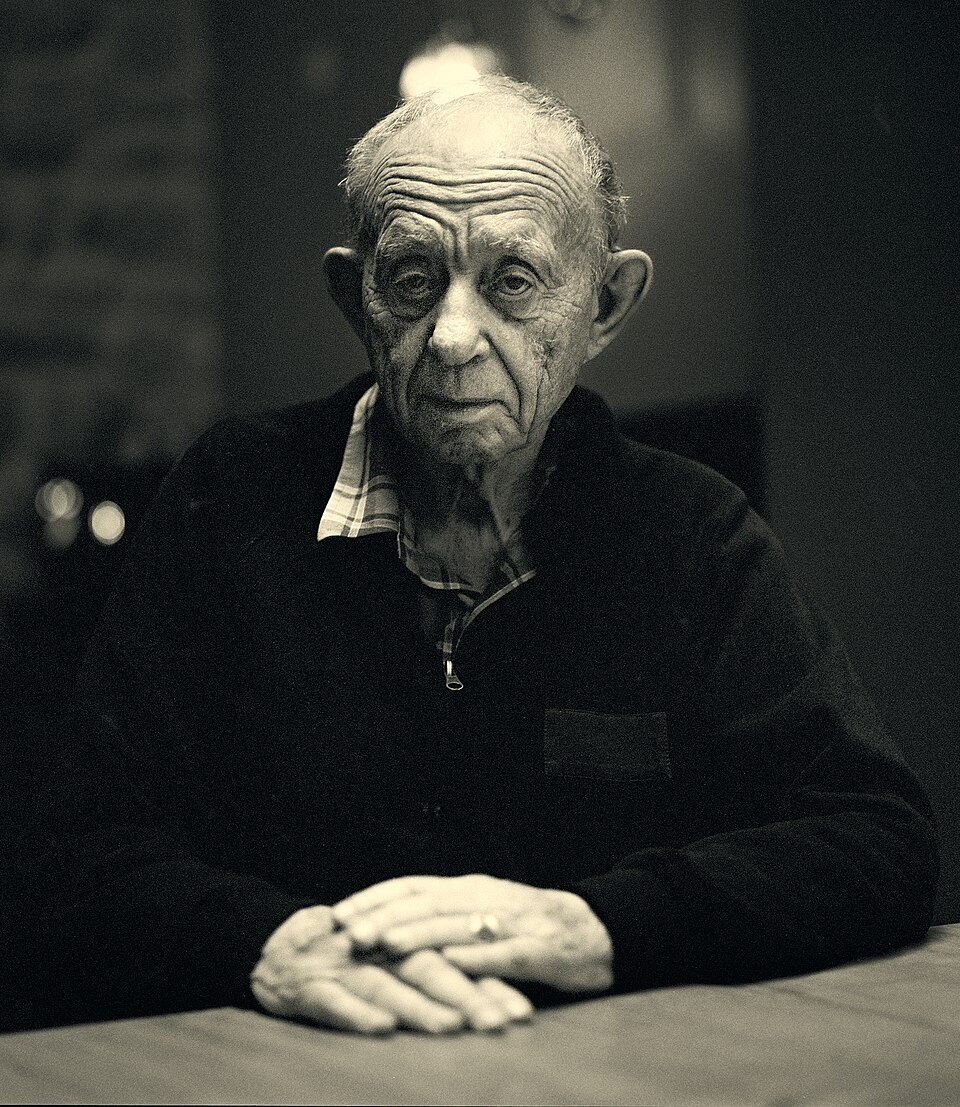
Kipnis, who holds a distinguished professorship in pathology and immunology at WashU Medicine, is co-director of the new MIND Center, a collaboration between WashU and the Weizmann Institute of Science in Israel. “These are some of the most complex and exciting questions in biomedicine,” he continues. “The nervous system, the immune system, and this whole world living within us—how do these three most complex systems talk to each other?”
And they do talk; they chat incessantly. The immune system is always surveilling the gut’s bacteria, looking for danger. The brain is always reacting to the immune system’s alerts.
“I can’t think of a single neurological or psychiatric condition where the immune system is not playing a role, at least secondary if not primary,” Kipnis remarks. Overall, he wants to learn, through the new center’s work, “how we can age and stay healthy.” But his specific focus is training the immune system to alleviate Alzheimer’s disease and ALS.
In 2001, Dr. Robert Schreiber (then, and still, on WashU’s faculty) identified the role the immune system plays in either shaping the development of tumor cells or destroying them. His research made it possible to use the immune system to target and destroy cancer cells.
Kipnis wants to do the same with neurodegenerative diseases, starting a step earlier.
“Your microbiome trains your immune system to know what is good and what is bad,” he explains. “If the microbiome is deficient, the immune system won’t be well trained. Can we train the immune system, engineer it maybe, with completely new cells that will go to the brain and do what we want them to do? And can we teach them to limit the inflammation to that particular area, so there are not all these side effects?”
In early Alzheimer’s, the microglia (immune cells that live in the brain) help us by eating plaques, slowing the disease’s development. But by the time the disease has reached its endstage, “the microglia are exhausted and angry, and they start eating not just the plaques but the neurons.” So how do you rejuvenate the microglia? Is the microbiome perhaps affecting how tired they get?
“The gut microbiome is mostly bacteria,” Kipnis says, stepping back to give a general overview. “We are living together in symbiosis with them, and we are all happy. We live in this beautiful synchrony with the gut microbiome. But you also have bugs, pathogens, that look very similar to the beneficial bacteria and can cause havoc with different organs. Now you need a full-blown immune response.”
And sometimes the immune system overreacts, while at other times, it is worn out.
“Think about an army,” Kipnis suggests. “When soldiers are rested, they do their job. But when they’re exhausted?” Friendly fire.
Other researchers at the MIND center will focus on different conversations within this gut-immune system-brain axis. Executive board member Dr. Jeffrey Gordon, who also holds a WashU distinguished professorship in pathology and immunology, is known as “the father of the microbiome.” His research has shown that by using special food to repair the gut microbiome of a starving infant or child, you can do far more than end malnutrition. You can start the development of a healthy immune system and alter the child’s predisposition to genetic diseases.
What have we learned, overall, about this gut-immune system-brain axis?
That beneficial bacteria in the gut help train and regulate the immune system, which then transmits messages to the brain and nervous system.
That imbalances in the gut microbiome can lead to an overactive immune response, contributing to inflammation.
That some bacteria produce molecules that can cross the blood-brain barrier themselves, like wily spies going behind the Iron Curtain. These bacteria do not need the intermediary immune system; they can affect brain function directly. “You cannot think crazier than nature has already thought,” Kipnis says dryly.
So what shapes our gut microbiome?
Genes, first. Your gut microbiome is unique to you, but its bacterial community will be more similar to that of a blood relative than to the community inside a stranger’s gut. That said, what you eat makes a significant difference. A junk food binge can change your microbiome in less than a day. Once you put away the SuzyQ’s and Cheese Puffs, your gut will restore its usual population. (And if you are supremely healthy, free of genetic predispositions, you can keep eating junk food without much consequence.)
But who among us is that healthy? And making permanent changes to the gut microbiome takes sustained effort—healthy food, sleep, exercise, all the wisdom we have ignored for millennia. People rolled their eyes at Ilya Mechnikov, winner of the 1908 Nobel Prize in medicine, for blathering about prebiotics and probiotics. He urged them to eat yogurt and drink kefir, which no doubt sounded strange in an era of aspic and blancmange. But he was right.
Other variables: Birth. (In mice born by C-section, the bacteria in the gut are less diverse than they are in mice born vaginally, because key bacteria are acquired during passage through the birth canal.) Stress hormones, heavy use of antibiotics, and various environmental toxins (pollution, pesticides, microplastics) can harm the microbiome; adequate sleep and exercise can support it. Even latitude makes a difference, Kipnis says: “Some diseases are very much dependent on where you live”—far north, with long winters and short days, or closer to the sunny equator, where there is very little multiple sclerosis or rheumatoid arthritis.
How secure is the funding for this research?
“There is no such thing as funding security,” Kipnis says. “But I do believe the current Administration understands—or will understand soon—that science is what brings the best and brightest people from around the world to this country. It’s one of the drivers of the economy, and of success, and America is leading the world. I do not think the Administration will let us lose that advantage.”
The puzzle he cannot fathom is more widespread: “When did science become the enemy of the American people, and why? What did we do that we lost that trust?
“People will say, ‘Why should I pay my tax money to study the genes of flies?’” he continues. “Well, a guy was studying glowing bacteria in the Arctic, and he realized that they have this channel that responds to blue light. Someone at Stanford put those channels on neurons, and now we can use blue light to turn neurons on and off. That guy at the North Pole never thought those glowing bacteria would ever be used in neuroscience. So if you have a choice about where you want your tax money to go, basic research is the place to strengthen.”
Read more by Jeannette Cooperman here.