The Rise and Fall of a Noble and Needed Black Institution
A local physician reviews Candace O’Connor’s history of Homer G. Phillips Hospital.
By Will Ross
March 22, 2022
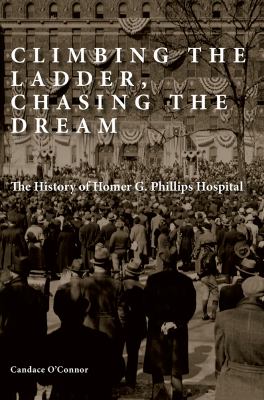
Climbing the Ladder, Chasing the Dream: The History of Homer G. Phillips Hospital
The story of the Homer G. Phillips Hospital in St. Louis is a deeply American one; a story that lays bare the moral conflict of a country that espouses human dignity and American exceptionalism, while denying fundamental services to its disadvantaged citizens on the basis of their skin color. It is a story of hope, pathos, sacrifice, and tragedy. It is a story of this country’s virulent racial prejudice, and the unwavering, uncompromising movement in St. Louis to provide high-quality health care to African Americans and other vulnerable groups. It is a story that needs to be told, and needs to be heard. That is a high charge to be placed on any established writer or historian who feels compelled to chronicle the transformative events leading to the inspiring opening of the Homer G. Phillips Hospital in 1937, and to its ignoble closing in 1979. Fortunately, for the sake of history and our posterity, veteran writer Candace O’Connor capably imparts that history and presents a series of powerful, passionate narratives in her new book, Climbing the Ladder, Chasing the Dream: The History of Homer G. Phillips Hospital.
In 1932, there was only one Black hospital for every 100,000 Blacks (or one hospital bed for every 1,000 Black patients). For Whites, it was one to 19,000 ratio (or one hospital bed for every 110 White patients). This statistic was particularly acute in St. Louis, which operated one public hospital, City Hospital #1, which remained segregated until 1964.
O’Connor captures the prevailing sentiment of African Americans in St. Louis during the period of the Supreme Court’s Plessy v. Ferguson’s separate but unequal ruling, and the rampant, de facto segregation and discrimination leading to a myriad of health disparities and lowered life expectancy among Blacks. Communicable diseases such as tuberculosis, and chronic diseases such as diabetes mellitus ravaged the African-American community, which was unable to obtain appropriate care at the segregated City #1 hospital and other predominantly White-run health institutions. The plight of African Americans at the turn of the twentieth century was made worse by the dearth of African-American health professionals, who had seen their ranks further diminished after the report by Abraham Flexner in 1910, which shuttered a disproportionate number of Black medical institutions. In his report Flexner noted: “Of the seven medical schools for negroes (sic) in the United States, five are at this moment in no position to make any contribution of value to the solution of the [Negro health] problem above pointed out. They are wasting small sums annually and sending out undisciplined men, whose lack of real training is covered up by the imposing MD degree.”
In 1932, there was only one Black hospital for every 100,000 Blacks (or one hospital bed for every 1,000 Black patients). For Whites, it was a one-to-19,000 ratio (or one hospital bed for every 110 White patients). This statistic was particularly acute in St. Louis, which operated one public hospital, City Hospital #1, which remained segregated until 1964. There were many unsung heroes who advocated for a hospital in the African-American community, but prominent attorney and civil rights activist Homer G. Phillips emerged as the movement’s legal mind and most ardent supporter. While city leaders argued for the construction of a Black facility linked to City Hospital #1, Phillips found that solution tantamount to “segregation with humiliation.” Phillips shepherded an $87 million city bond issue, of which $1 million would be allocated for the creation of an African-American hospital. That bond issue passed in 1923, but the construction and opening of the Homer G. Phillips hospital would be delayed until 1937. Phillips, whose murder in 1931 was never fully resolved, would not live to see the opening of the hospital. The St. Louis community memorialized him by naming the hospital in his honor.
O’Connor also recognized the cultural importance of locating the Homer G. Phillips Hospital in the African-American community called the Ville in the City’s Northside. The Ville, home of several institutional icons including Sumner High School, Annie Malone Children’s Home, Poro College, and Antioch Baptist Church, had a thriving social and economic center due to a strong African-American middle-class, spurred by the Great Migration of African Americans from the Deep South. Woven throughout the book are heartwarming narratives from individuals who lived and worked in the Ville neighborhood, including author and historian John A. Wright Sr., whose mother also worked at Homer G. Phillips Hospital. Dr. Wright’s portrayal of the Ville, along with imagery created by former nurses and members of the community, reminded us of the paradox of segregation—the time when prominent African-American business owners, lawyers, physicians, teachers, clergy, and others, whose mobility was constrained by harsh restrictive covenants, resided in a Black community where they created strong social networks, provided social and economic support, and contributed to the vitality of the neighborhood, not unlike Tulsa’s Black Wall Street. The Homer G. Phillips Hospital, a majestic seven-story Art Deco-style building, would not only be a source of healing and caring for the community; it would also spawn hundreds of jobs that further stabilized the Ville neighborhood.
There were many unsung heroes who advocated for a hospital in the African-American community, but prominent attorney and civil rights activist Homer G. Phillips emerged as the movement’s legal mind and most ardent supporter.
Did the hospital live up to its expectations as a mecca for Black health care? According to O’Connor, it was truly “a first-class place.” (156) Recognizing that the eyes of the world were upon them, Dr. William Sinkler, head of surgery from 1956 and the medical director from 1941 until his death in 1960, imposed exacting standards on the professional staff. Dr. Robert Elman, professor of clinical surgery at Washington University School of Medicine and head of surgery at Homer G. Phillips Hospital, provided unwavering support to Dr. Sinkler, and was renowned for his teaching and mentoring of Homer G. Phillips’s residents and nursing staff. Both men also had a strong sense of social justice and were quite aware of the “historical moment” in which they operated. The hospital quickly developed the reputation as the place to go if you were shot or stabbed, because the chances of survival were so much better. The community tagline, spoken with immense pride, was “take me to the G.” By 1950, 620 residents and 479 nurses had been trained at the hospital, and three-quarters of African-American babies were born at Homer G. Phillips. In its heyday, one out of three African-American physicians in the country were trained at Homer G. Phillips Hospital, including such luminaries as Drs. LaSalle Lefall, James Whittico, Frank Richards, Howard Venable, and Helen Nash.
The success of O’Connor’s book comes not just from the gripping tales of St. Louis politics, with its palpable racial overtones, but from the personal recollections of the hospital’s staff and community leaders, who viewed the hospital with awe and reverence. One of the most moving parts of the book is the segment on the nurses, who were the consummate angels and backbone of the hospital. Many of the nurses left impoverished communities in the South and sought professional and economic opportunities at Homer G. Phillips Hospital. Like the unforgettable characters in Isabel Wilkerson’s epic, ethnographic masterpiece, The Warmth of Other Suns, the nurses moved to St. Louis, where, according to novelist Richard Wright, they could transplant their dreams “in alien soil.” Under the caring but strict supervision of nursing supervisors Mabel Northcross, and later Minnie Gore, the nurses exceeded the standards set for them and never missed a beat, from treating patients with multiple gunshot wounds to finding an apartment for a new mother who was living in an unheated garage. As the hospital was facing closure in the late 1970s, members of the Homer G. Phillips Nurses Alumni Association were on the front lines advocating for the hospital’s future, reminding the public of the hospital’s remarkable legacy and the pressing need for a medical institution of its caliber in North St. Louis.
The community tagline, spoken with immense pride, was “take me to the G.” By 1950, 620 residents and 479 nurses had been trained at the hospital, and three-quarters of African-American babies were born at Homer G. Phillips.
Homer G. Phillips hospital, under insurmountable duress, closed its operations in August 1979. The factors contributing to its closing, including overt racial hostility, will be debated for decades to come. O’Connor does not pull any punches in calling out the White political leadership’s shortsightedness and lack of moral fiber in allowing the facility to close. Its closure left a gaping hole in the African-American community, contributing to the poor health status of residents in North St. Louis and the demise of the Ville neighborhood. African Americans in St. Louis categorically cite the closure of the hospital as a persistent source of racial animosity and distrust of current White health care institutions. Many esteemed public hospitals serving the African-American community closed in the twentieth century, however none were as treasured or impactful as the Homer G. Phillips Hospital. While even longstanding wounds can be healed, healing must begin with the recognition of the insult and a path forward that offers restorative justice. In St. Louis, Missouri, that healing begins with extolling the history of the legendary Homer G. Phillips Hospital.